Advocate now to ensure food allergy is taken into consideration for the proposed pan-Canadian school food policy by participating in a consultation. Learn about the immune response and how it can help inform food allergy treatments, plus discover the different food allergy therapies and the trials underway globally. Participate in a birch allergy study and take part in an international survey on food allergy and airline travel. Plus, check out our mythbuster about whether someone with a tree nut allergy should avoid peanuts.
Advocacy in action: Ensure that food allergy is taken into consideration for the proposed pan-Canadian school food policy
Participate in Government of Canada’s online consultation on building a pan-Canadian school food policy. The deadline to participate is December 16th, 2022.

With the current economic conditions in Canada, the need for a comprehensive school food policy has never been greater. Many children go to school on empty stomachs and many families cannot reliably access sufficient nutritious foods. To address this important need, the Government of Canada’s Department of Employment and Social Development is proposing the development of a national school food policy to address the needs of students across the country.
Canadian families managing food allergy report higher rates of food insecurity compared to families who do not manage food allergy, and the rates of severe food insecurity have increased for these food allergy families since 2019.
This means that many Canadian families that manage food allergy are unable to purchase safe, nutritious foods. A comprehensive national school food policy may benefit children with food allergy in our schools.
The government is now gathering input into what priorities should be considered when implementing this policy. Your voice is needed to help ensure that accommodations for food allergy are included in any proposed national school food policy.
Here’s what you need to know:
The government’s goals for a pan-Canadian school food policy specifically address the need for all children to have access to safe, nutritious food and to reduce poverty and food insecurity. The themes that have been identified for this policy include:
- Improve access to school food and mitigate financial barriers
- Prevent stigma
- Enhance nutrition and promote lifelong healthy practices
- Ensure a flexible approach that leaves room for local adaptation
- Offer culturally appropriate programming that is mindful of dietary requirements
- Ensure accountability and governance
- Supporting local and sustainable food systems and economies
Food Allergy Canada supports these objectives and measures to help provide safe, nutritious food options for all children, including those impacted by food allergy.
Next steps: Participate in the consultation
You and all Canadians with food allergy an opportunity to have your voice heard for how food allergy may be managed within a school food policy. Please participate in this consultation.
Take these steps:
- Read the discussion paper.
- You are encouraged to read the discussion paper before completing the questionnaire. It provides background information on school food programs and possible guiding principles for a school food policy.
- Complete the consultation questionnaire by December 16, 2022.
- The questionnaire takes around 10-15 minutes to complete.
- Share this link with others in your community that would be interested in participating in this consultation
Thank you in advance for your support in helping to make an impact and drive change!
Science corner: Immune mechanisms of food allergy and ties to therapy
The immune response and how it can help inform treatments for food allergy is summarized in this article from Allyssa Phelps and Joshua F.E. Koenig, Ph.D. – Researchers at the Schroeder Allergy and Immunology Research Institute at McMaster University.
Read below to find out about the different food allergy therapies and the trials underway globally.
Food allergy and the immune system
Food allergy occurs when our immune system makes antibodies called IgE antibodies against food. When someone eats the food to which they are allergic, IgE antibodies cause cells called mast cells to immediately release molecules that cause allergic reactions. The goal for therapies in food allergy is to stop making IgE against foods. In some people, the immune system “forgets” how to make IgE antibodies against the food they are allergic to, and they outgrow their allergy. Researchers are still working to figure out how exactly that happens.
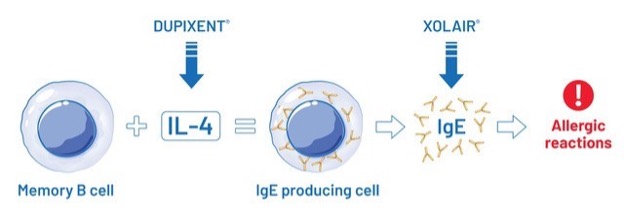
The immune system “remembers” to stay allergic because of cells called memory B cells. Memory B cells do very little other than staying quiet, waiting, and remembering. When someone with food allergy is exposed to their food allergen, memory B cells wake up and become cells that make IgE antibodies. Memory B cells need a molecule called IL-4 to become the cells that make IgE. This process is drawn out below.
New therapies for food allergy
Many research labs and pharmaceutical companies are testing new therapies for food allergy. Listed below is a table describing some therapies that are currently in clinical trial in the global network. These therapies include:
- allergen immunotherapies which involve providing increasing amounts of a food allergen to increase the amount that can be tolerated without a reaction,
- biologics which target specific biological pathways, and
- newer therapeutic approaches like vaccination and fecal transplant.
Currently, the protection provided by oral immunotherapy, also known as OIT, (a treatment that is currently being conducted in Canada under CSACI guidelines) is not permanent for most people. Patients must continue these treatments indefinitely or risk the allergy returning. Many researchers are trying to maximize the benefits of OIT by supplementing it with additional therapies; for example, biologics like XOLAIR and DUPIXENT which block specific biological pathways.
Further investigation of existing treatments and the development of new therapies is important to help find a cure for food allergy. This is especially important for patients who are allergic to multiple foods, or who have co-morbidities, where multiple immunotherapy products which are taken indefinitely would be required.
| Drug/Therapy | Objective/Mechanism | Impact | Status in testing |
|---|---|---|---|
| XOLAIR | Eliminates levels of IgE circulating in the body | Eliminates allergic reactions while patients are on therapy | Currently in clinical trials |
| DUPIXENT | Targets the receptors that detect IL-4, which stops memory B cells from becoming IgE producing cells | Increases the amount of allergen that can be safely eaten | Discontinued clinical trials; did not increase the amount of allergen that could be safely eaten |
| PALFORZIA® (Oral immunotherapy) | Peanut is given orally in increasing doses, up to a maintenance dose that is tolerated | Increases the amount of allergen that can be safely eaten | Approved by the U.S. FDA |
| DUPIXENT + PALFORZIA | Block IL-4 when memory B cells are “woken up” by allergen | Increases the amount of allergen that can be safely consumed, reduces side effects | Currently in clinical trials |
| Sublingual immunotherapy (SLIT) | Food allergen is given under the tongue at a maintenance dose that is tolerated | Increases the amount of allergen that can be safely eaten, fewer side effects than (OIT) | Currently in clinical trials |
| Epicutaneous immunotherapy (EPIT) | Patch containing a food allergen is applied to the skin for increasing periods of time | Increases the amount of allergen that can be safely eaten | Currently in clinical trials |
| Vaccinations | Re-direct the existing allergic response against the food (peanut) towards a safe immune response | May reprogram the immune system | Currently being studied in clinical trials |
| Fecal transplantations | Replaces the unhealthy gut microbes that have been identified in allergic people with healthy gut microbes | Increases the amount of allergen that can be safely eaten | Currently in clinical trials |
Table contains food allergy therapies that are currently being tested.
Do you have a question about the science behind these therapies for the researchers? If so, send it to us at info@foodallergycanada.ca and we may feature it in an upcoming newsletter.
Research: Participate in a birch allergy study – registration extended to January

A birch allergy study is underway at Cliantha Research in Mississauga, Ontario. They are seeking healthy adults to participate in this study.
As there is cross-reactivity with birch pollen and certain fresh fruits, vegetables and tree nuts, some members in the food allergy community who may also have a birch allergy might be interested in this study or know affected individuals who could be interested.
Learn more, including eligibility and compensation for participants.
Research: Participate in an international study on food allergy and airline travel
A global research team led by Northwestern University is conducting a study to learn more about air travel experiences by people with food allergy. Have your say by completing the survey, and please share with others.
Mythbuster – If someone has a tree nut allergy, should they avoid peanuts?

Read our mythbuster to understand the differences between tree nuts and peanuts.
Plus, stay tuned for the recording of our December 8th tree nut allergy webinar to learn the latest in allergy management and test yourself on how well you can identify one nut from another.
Help us educate your communities and share this mythbuster with them! Find more mythbusters at foodallergycanada.ca/mythbusters.
Tags: advocacy, consultations, mythbusters, peanuts, Research, science corner, tree nuts
